is apparently not enough to keep the doctors away.
But, here is James, his first apple in two years.
His Apple History:
He reacted to a fruit salad (no apple) on June 30, 2014, the day before his 12th birthday. He had a two system reaction and so self administered his epi-pen. Later that summer, he got an itchy mouth when eating apple, although he had applesauce earlier that day with no reaction. This disparity led his allergist to test him for oral allergy syndrome (OAS). In one of those weird twists, he did not test positive for apple (on the fresh apple skin test, no IgE was taken). However, he tested positive for other fruits and vegetables, including the melon that we now know caused his reaction.
His allergist advised me that we could do an at home challenge for apple. However, at the time, he was having issues with more and more foods and we were in the process of simplifying his diet. He had no desire to try apple. Since he could eat most apple products, just not fresh apple, we left it alone.
Fast Forward:
He has improved immensely, both physically and emotionally. His IgE for grasses, which is what causes his OAS allergies, are now nearly negative (0.24 and 0.37, a 90% and 89% reduction). We are joining friends this weekend on a hike followed by apple picking; he wanted to be able to eat an apple.
So, we decided to go ahead with the challenge recommended two years ago.
Please note: I am not giving medical advice or recommending you follow these steps. I am describing the steps recommended only in this particular case by a board certified allergist. If you have questions specific to you or your child, please consult your own board certified allergist. Thank you.
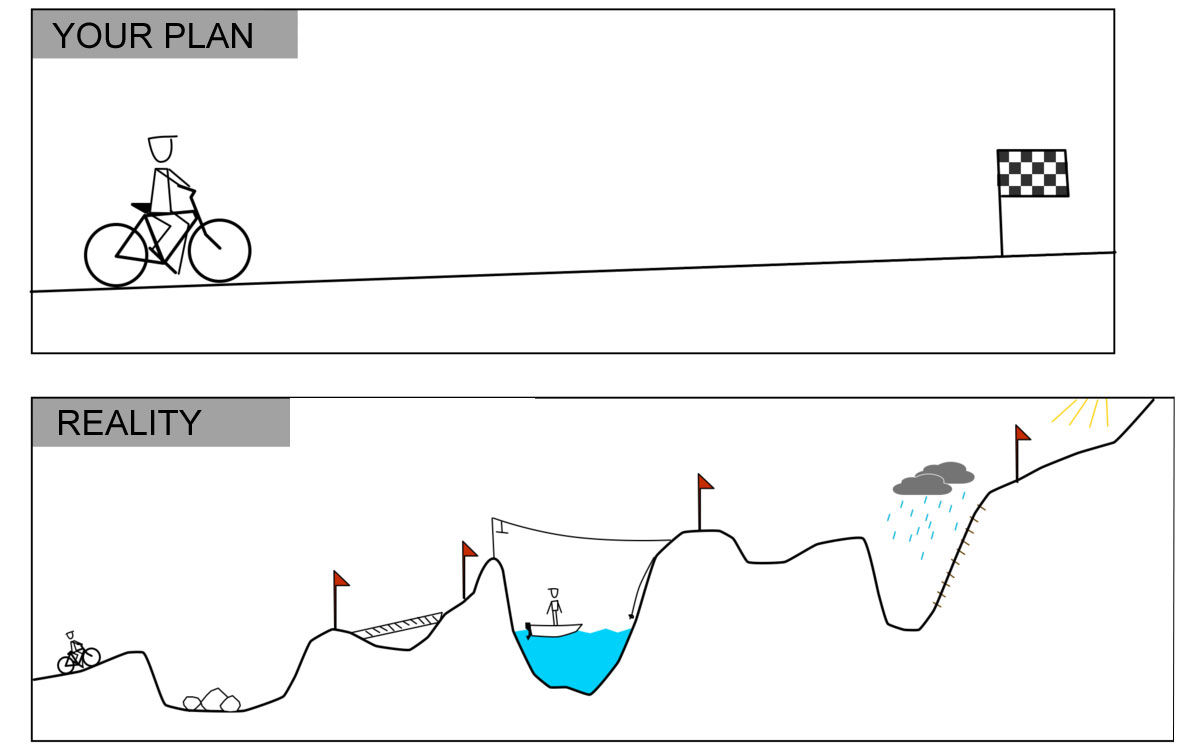
What was supposed to happen:
1. Take a thin slice of apple, put it to his lips, wait 15 min.
2. Microwave a small slice of apple for 10 sec. Take a nibble. Wait 15 min.
3. Slowly finish the microwaved slice over 15 min. intervals.
4. Repeat with a fresh slice.
5. Continue eating more until an entire apple has been eaten.
What did happen:
1. Hand James the apple slice to put to his lips.
2. He eats before I can say anything.
3. "What, was I not supposed to eat it?"
The results:
The first day he tried apple (about half of the entire apple), he got some very minor digestive problems. This is not entirely out of the ordinary for him and he was likely nervous. So, we stopped for the day and said we would come back to it.
Two days later, he finished an entire apple with no symptoms. And just like that, one food is down.
Moving Forward:
I plan to celebrate this victory for a while before moving forward. Whether he never had OAS to apples or he if his environmental allergies improved enough that he can now tolerate it, it is a victory. He is confident enough that he will try foods he has been avoiding.
The next food I plan to re-introduce is green beans. His allergist also felt that his issue with legumes is more of an intolerance. Legumes are histamine liberators. Since he has had a histamine type reaction, it is possible that, while his body was recovering from a reaction in particular, he had trouble digesting them. I will not be home trialing any that he was specifically tested for (all were positive) without discussing with his allergist. But, I am ready to lift the "avoiding legumes" label if possible.
Update:
In perfect irony, James got sick, so we will not be going apple picking this weekend. Nothing to do with apples or allergies, just your standard virus. Considering that in two years, he has not had a fever ever, I am debunking the "apple a day keeps the doctor away" advice.